Midwifery Musings: What to Expect During Your Third Trimester
Covington Women’s Health Specialists midwife, Jennifer Walker, CNM, returns with more thoughtful guidance in the latest installment of our Midwifery Musings blog series. With her firsthand experience supporting patients through every step of pregnancy, Jennifer offers a closer look at what to expect during the third trimester and how our care team supports you as delivery day approaches.
If you’re just joining the series, be sure to review our previous posts covering the pregnancy confirmation visit, your initial prenatal exam, and what to expect in the second trimester.
Welcome to the final stretch! The third trimester spans from week 28 to delivery, typically around week 40. It brings exciting milestones as you prepare to meet your baby. During this time, your prenatal visits and screenings become more frequent as your care team closely monitors both your health and your baby’s development.
Your 28-Week Appointment and Third Trimester Testing
At your 28-week appointment, plan to spend at least an hour in our office. This visit includes important tests to ensure a healthy pregnancy:
- Glucose Screening Test: This one-hour test checks for gestational diabetes. (No need to fast beforehand. It’s important that you can eat before your appointment!)
- Blood and Urine Tests: These help monitor for signs of anemia and infection.
- TDaP Vaccine: Recommended by the American College of Obstetricians and Gynecologists, this vaccine helps protect your baby from pertussis (whooping cough).
- RhoGAM Injection: If your blood type is Rh-negative (such as O-, A-, B-, or AB-), you’ll receive a RhoGAM shot to prevent complications from Rh incompatibility.
If anything in your test results or symptoms needs closer attention, your provider may order additional tests or ultrasounds to evaluate your baby’s growth, amniotic fluid levels, or placenta.
From Biweekly to Weekly Visits
After your 28-week appointment, you’ll begin seeing your provider every two weeks. Once you reach 36 weeks, those visits become weekly. At your 36-week appointment, we’ll perform two vaginal swabs:
- Group B Strep (GBS): This common bacteria isn’t harmful to you but can pose risks to your baby during delivery. If you test positive, we’ll provide prophylaxis antibiotics during labor to protect your baby.
- STD Screening: As recommended by the CDC, we screen all patients for chlamydia and gonorrhea at this stage.
You’ll also sign a delivery consent form at this visit whether you’re planning a vaginal or cesarean birth. Your provider will walk you through the details and answer any questions you may have about your birth plan.
What Comes Next
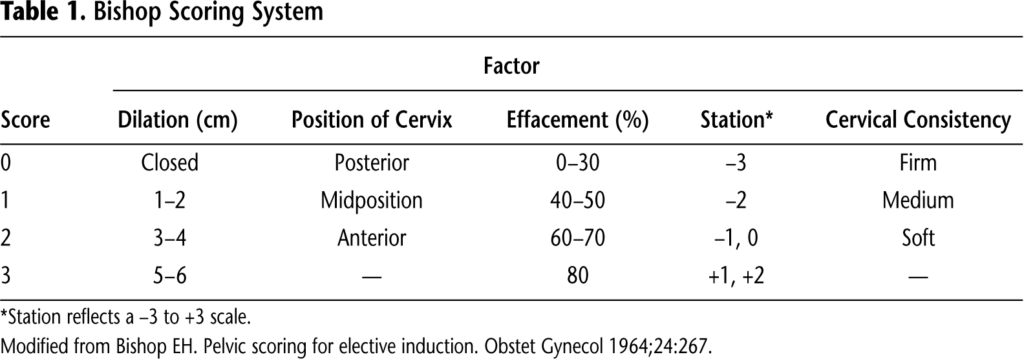
Starting at 37 weeks, cervical exams become available to assess dilation, but they’re entirely optional. Keep in mind that every pregnancy is unique, and your care plan, testing, and ultrasounds will be tailored specifically to you.
The third trimester can feel overwhelming, but it’s also a time of great anticipation. At Covington Women’s Health Specialists, we’re proud to partner with you during this exciting phase and are here to provide evidence-based guidance, compassionate support, and shared decision-making throughout your pregnancy journey.
We look forward to walking with you through these final weeks, along with celebrating the arrival of your newest family member! If you have any questions or concerns, give us a call (770) 385-8954, or request an appointment online.